Indice
- 1. Pathogenesis
- 2. Clinical manifestations
- 3. Diagnosis
- 4. Treatment and prognosis
Immune Thrombocytopenia (ITP) in children
Malattie Delle Piastrine
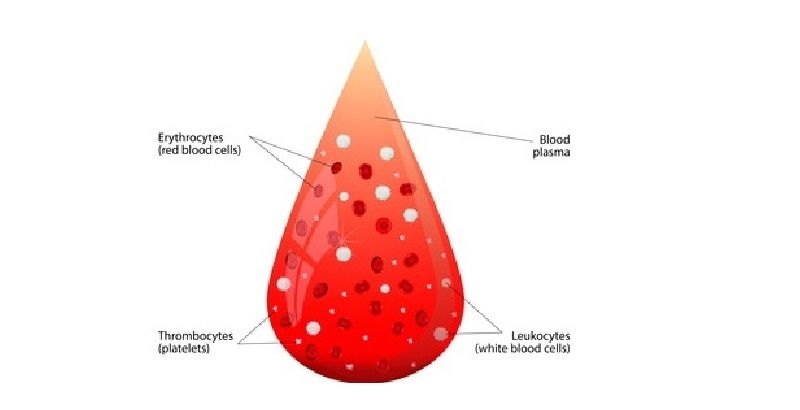
Immune thrombocytopenia of children is characterized by isolated thrombocytopenia with a platelet count < 100,000/mcL and normal white blood cell count and normal hemoglobin. The cause of ITP remains unknown in most causes. It can be initiated by a viral infection or other immune trigger. (1) (Journal of Pediatric Hematology/Oncology 2013 vol. 35 pp. 1-13) ITP in children normally resolves spontaneously within 3 months and only few children will have persistent ITP that is defined as thrombocytopenia and symptoms lasting more than 3 months but less than 12 months. About 20% of children with ITP will develop chronic ITP that is defined as thrombocytopenia lasting more than 12 months. (2) (Blood 2010 vol. 115 pp. 2386-2393) ITP in absence of other causes or disorders that can be associated with thrombocytopenia is primary ITP. On the contrary, secondary ITP is an immune thrombocytopenia associated with the use of some drugs, with HIV, with systemic lupus erythematosus (SLE), common variable immunodeficiency (CVID) and hepatitis C. The annual incidence of ITP in children is estimated to be between 1 and 6,4 cases per 100,000 children. ITP typically presents with the sudden appearance of a petechial rash, bruising, and/or bleeding in a child who, except for these symptoms, is healthy.
As initial laboratory evaluation must be performed a complete blood count (CBC) and peripheral blood smear, a reticulocyte count, a direct antiglobulin test (DAT) and a dosage of immunoglobulins.
A bone marrow examination is not required in children with a typical presentation and laboratory findings of ITP. Bone marrow aspiration and eventual biopsy are recommended in case of atypical clinical or laboratory characteristics at presentation, if during follow-up the patient presents new findings that are not typical of ITP, in case of treatment failure.
Treatment may be a watchful waiting or a pharmacologic intervention. Pharmacologic options include intravenous immunoglobulin (IVIG), intravenous anti-D immune globulin (anti-D), or glucocorticoids as initial treatment that must be started in children with severe or life-threatening bleeding according to the guidelines published by the American Society of Hematology (3) (Blood 2011 vol. 117 (16) pp. 4190-4207) and also in children with a platelet count < 10,000/mcL and signs of substantial cutaneous bleeding as extensive bruising, petechiae and in children with a platelet count < 30,000/mcL and signs of moderate bleeding as mucosal bleeding, epistaxis or hematuria. (4) (www.uptodate.com 2014)
In patients with chronic ITP, whose symptoms and risk are not controlled by standard therapy, we may use other therapies such as splenectomy and rituximab.Thrombopietin receptor agonists are not established treatments for children with ITP,in fact they have been used only in small case series.Large trials of romiplostim are in progress(clinicaltrials.gov/show/NCT01071954) (clinicaltrials.gov/show/NCT01444417) and eltrombopag is investigated in other two trials (clinicaltrials.gov/show/NCT00908037) (clinical trials.gov/show/NCT01520909). Preliminary results indicate that these agents have the same efficacy and safety demonstrated in adult patients.
Recently at the 56th Annual Meeting of the American Society of Hematology in December 2014 was presented a study of 40 pediatric patients with Immune Thrombocytopenia treated with Romiplostim in a long-term extension study up to 4.2 years and platelet counts in pediatric patients with chronic ITP were maintained without significant toxicity. No bone marrow biopsies were performed and no thrombotic events were reported. (5) (Blood 2014 (21) Abstract 4184) see section on "Treatment and prognosis".
References :
1 ) D’Orazio J.A., Neely J., Farhoudi N. et al. : ITP in children : pathophysiology and current treatment approaches. Journal of Pediatric Hematology/Oncology 2013; 35 : 1-13
2 ) Rodeghiero F., Stasi R., Gernsheimer T. et al. : Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children : report from an international working group. Blood 2009; 113 : 2386-2393
3 ) Neunert Cindy, Lin Wendy, Crowther Mark et al. : The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood 2011; 117 (16) : 4190-4207
4 ) Bussel James B., Mahoney Donald H., Hoppin Alison G. et al. : Immune Thrombocytopenia (ITP) in children : Initial management. www.uptodate.com 2014
5 ) Bussel James B., Tarantino Michael DE., Geddis Amy et al., : Safety and efficacy of long-term open-label dosing of Romiplostim in thrombocytopenic pediatric patients with immune thrombocytopenia. Blood 2014 (21) Abstract 4184
www.blooodjournal.or/content/124/21/4184